 By Independent News Roundup
By Independent News Roundup
For years, COVID-19–vaccinated people have collapsed or died suddenly with “no explanation” — athletes on the field, young adults in their sleep, and otherwise healthy individuals with no prior heart history. Our new peer-reviewed paper titled, COVID-19 Vaccine-Induced Subclinical Myopericarditis: Pathophysiology, Diagnosis, and Clinical Management, published in the European Society of Medicine’s Medical Research Archives, finally connects the dots — and provides real solutions.
A silent epidemic of subclinical myopericarditis and heart injury is occurring beneath the surface — often without symptoms, without warning, and in some cases, with sudden cardiac arrest as the first sign of disease.
This is the first peer-reviewed paper to formally define, characterize, and clinically map COVID-19 vaccine-induced subclinical myopericarditis. We establish the first unified diagnostic and risk-stratification framework for identifying subclinical cases — and present the first structured management and detoxification protocol aimed at reducing ongoing Spike-mediated cardiac injury.
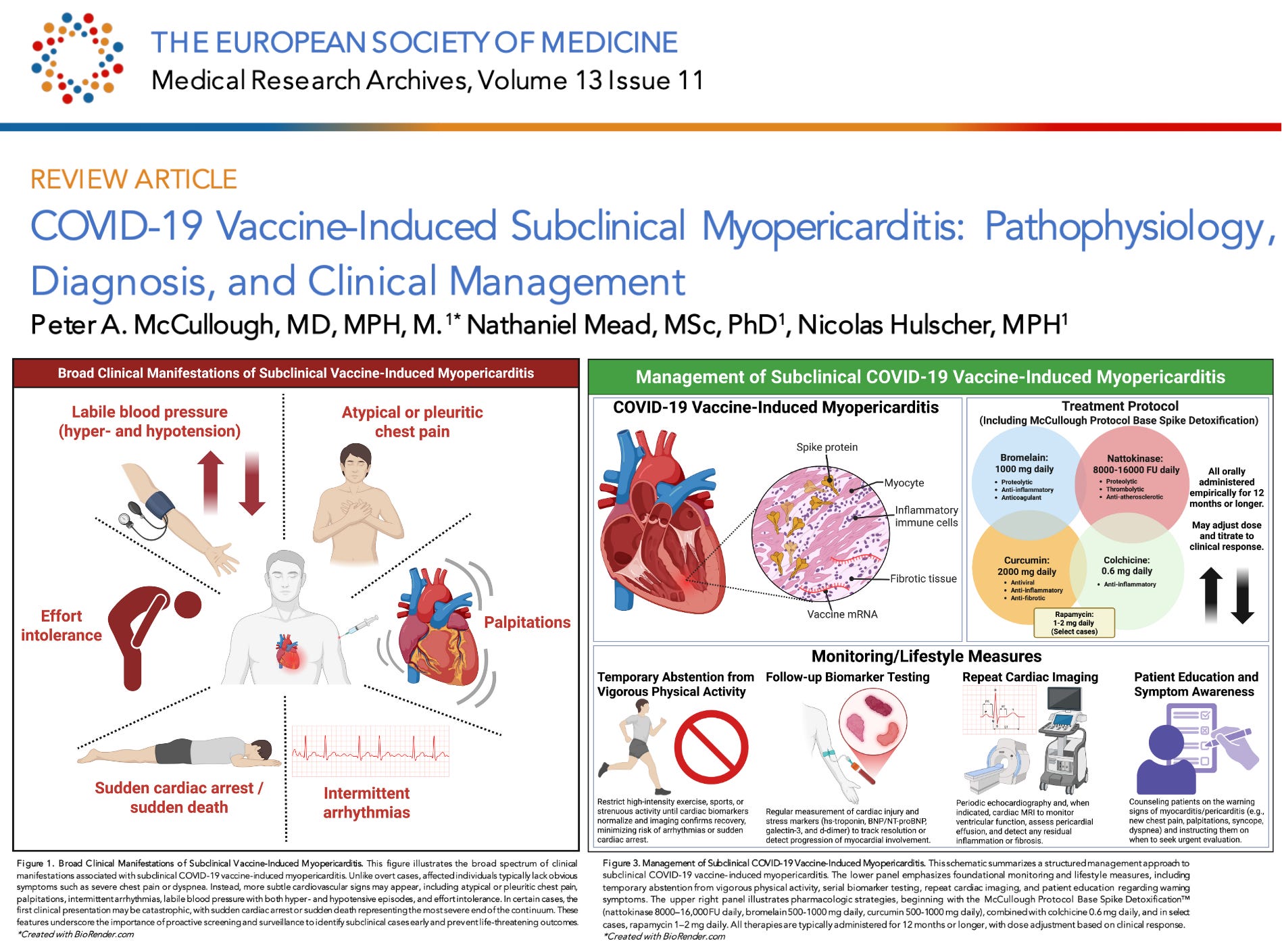
Subclinical myopericarditis is heart inflammation caused by COVID-19 mRNA vaccination that occurs without the classic warning signs seen in overt myocarditis. Instead of dramatic chest pain or hospitalization, the injury unfolds silently — detectable only through biomarkers, ECG changes, imaging, or antibody/spike measurements.
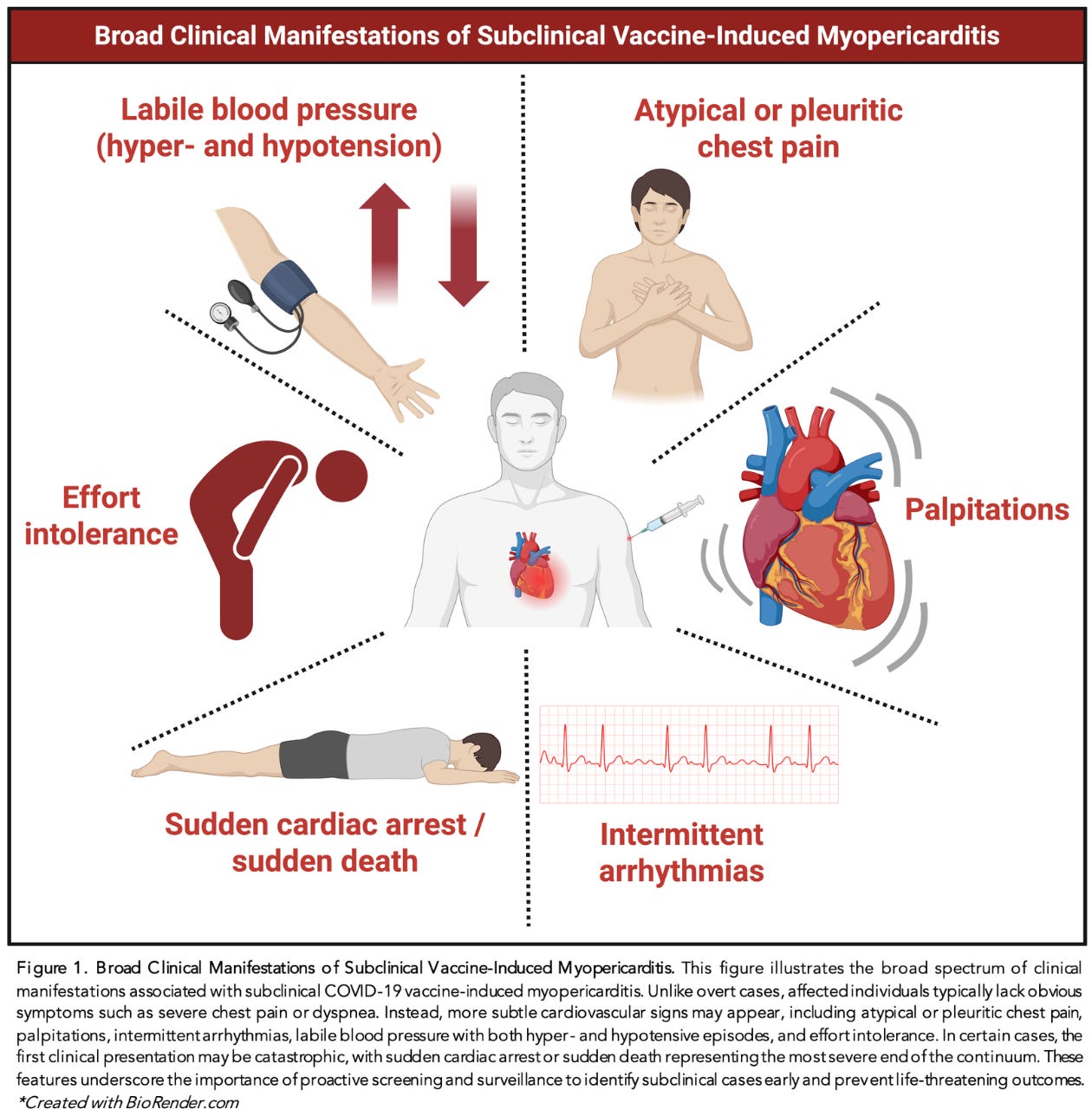
Unlike traditional myocarditis, which presents with obvious symptoms, subclinical vaccine-induced myopericarditis:
Because affected individuals appear outwardly healthy, this condition is vastly underdiagnosed.
The spectrum of subclinical myopericarditis is broader — and more dangerous — than the public has been told. Based on the evidence synthesized in the paper, individuals may experience:
In some individuals, the initial manifestation may be catastrophic: Sudden cardiac arrest without any prior symptoms.
Autopsy studies show microscopic inflammatory scars too small for MRI to detect, yet fully capable of triggering lethal arrhythmias.
The emerging evidence suggests that silent heart damage after mRNA vaccination is far more common than health authorities acknowledged. Based on prospective studies and symptom surveillance, a meaningful percentage of recipients — especially younger individuals — may have experienced measurable myocardial injury without ever knowing it. As we outline in the paper:
“The incidence of subclinical myopericarditis is challenging to estimate, as it requires sensitive screening and is not associated with symptoms that would prompt clinical evaluation. Chiu et al found among 763 students a rate of 17.1% had at least one cardiac symptom after the second vaccine dose, mostly chest pain and palpitations. Three prospective cohort studies have evaluated the incidence of subclinical myopericarditis after injection of synthetic mRNA. Mansanguan et al. reported an incidence rate of 2.3%, Buergin et al. reported an incidence rate of 2.8%, and a Pfizer-sponsored study yielded an estimated incidence rate of 1.0%, though that study omitted daily cardiac troponin measurements. It is reasonable to surmise that approximately 1–3% of COVID-19 mRNA vaccine recipients suffer some degree of myocardial injury per dose, thereby representing a profound concern for the short- and long-term health of younger vaccinees.”
When applied across millions of doses, a 1–3% injury rate translates into millions of individuals with unrecognized cardiac damage — underscoring the urgent need to take subclinical myopericarditis seriously and to implement proper diagnostic and treatment pathways.
Our paper outlines the first structured clinical management pathway for subclinical myopericarditis following COVID-19 mRNA vaccination. This framework — summarized in Figure 3 of the publication — integrates lifestyle precautions, biomarker surveillance, imaging follow-up, and targeted pharmacologic intervention.
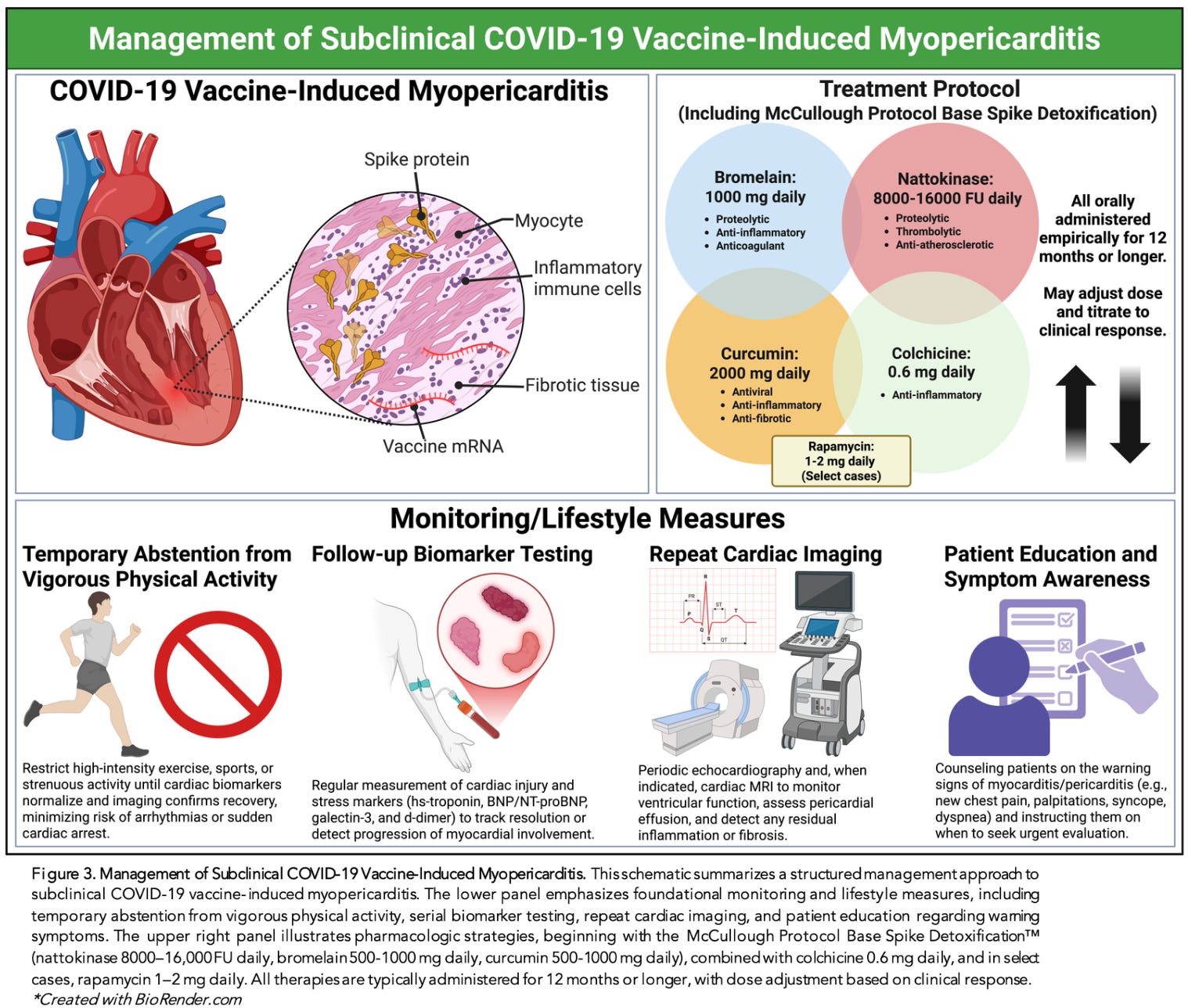
The first priority is to avoid exacerbating myocardial inflammation, prevent arrhythmic triggers, and track the trajectory of recovery. Recommended foundational steps include:
These conservative measures form the base layer of long-term care.
The second layer of management focuses on clearing persistent Spike protein, reducing inflammation, and preventing progression to chronic fibrosis or arrhythmic risk. The paper details a structured, multi-agent approach:
A targeted 3-part regimen designed to degrade circulating Spike protein and reduce inflammatory load:
These agents work synergistically to enhance proteolysis, modulate endothelial inflammation, and support microvascular recovery.
Evidence supports colchicine in reducing pericardial and myocardial inflammation. It is recommended for most moderate or persistent subclinical cases.
For prolonged or relapsing inflammation, rapamycin offers mTOR inhibition that can:
Its use is generally reserved for severe cases with documented ongoing myocardial involvement.
All components of management — lifestyle, monitoring, detoxification, and medications — are typically continued for 12 months or longer, with dosage and duration tailored to:
This recognizes the chronic nature of Spike persistence and the long healing times required for inflamed myocardium.
COVID-19 vaccine-induced subclinical myopericarditis represents a silent, widespread, and devastating form of cardiac injury. Countless indidvuals around the world are now living with undiagnosed heart inflammation — without obvious warning signs.
This paper finally gives clinicians the diagnostic tools, risk framework, and management strategies needed to identify and treat this condition. It closes a gap that should never have existed — a gap created by regulatory agencies that refused to investigate, refused to monitor, and refused to acknowledge the scale of vaccine-induced injury.
What the CDC should have done, the McCullough Foundation is doing.
For four years, regulators ignored the vaccine-injured and failed to develop any clinical guidance. The McCullough Foundation stepped in to fill the vacuum — conducting the research, publishing the papers, and building the pathways they would not. We will continue finding real solutions for the millions of vaccine-injured worldwide.
But this work depends on independent support. If you believe in this mission and want to help accelerate urgent research, clinical protocols, and public education, please consider donating to the McCullough Foundation: https://mcculloughfnd.org/products/donate-1
