 By Independent News Roundup
By Independent News Roundup
The single largest and most rigorous study ever conducted on vaccines and dementia — spanning 13.3 million UK adults — has uncovered a deeply troubling pattern: those who received common adult vaccines faced a significantly higher risk of both dementia and Alzheimer’s disease.
The risk intensifies with more doses, remains elevated for a full decade, and is strongest after influenza and pneumococcal vaccination. With each layer of statistical adjustment, the signal doesn’t fade — it becomes sharper, more consistent, and increasingly difficult to explain away.
And critically, these associations persisted even after adjusting for an unusually wide range of potential confounders, including age, sex, socioeconomic status, BMI, smoking, alcohol-related disorders, hypertension, atrial fibrillation, heart failure, coronary artery disease, stroke/TIA, peripheral vascular disease, diabetes, chronic kidney and liver disease, depression, epilepsy, Parkinson’s disease, cancer, traumatic brain injury, hypothyroidism, osteoporosis, and dozens of medications ranging from NSAIDs and opioids to statins, antiplatelets, immunosuppressants, and antidepressants.
Even after controlling for this extensive list, the elevated risks remained strong and remarkably stable.
The primary adjusted model showed that adults receiving common adult vaccines (influenza, pneumococcal, shingles, tetanus, diphtheria, pertussis) had a:
This alone dismantles the narrative of “vaccines protect the brain,” but the deeper findings are far worse.
Buried in the supplemental tables is a more shocking result: when the authors restricted analyses to Alzheimer’s disease specifically, the association grew even stronger.
This indicates the effect is not random. The association intensifies for the most devastating subtype of dementia.
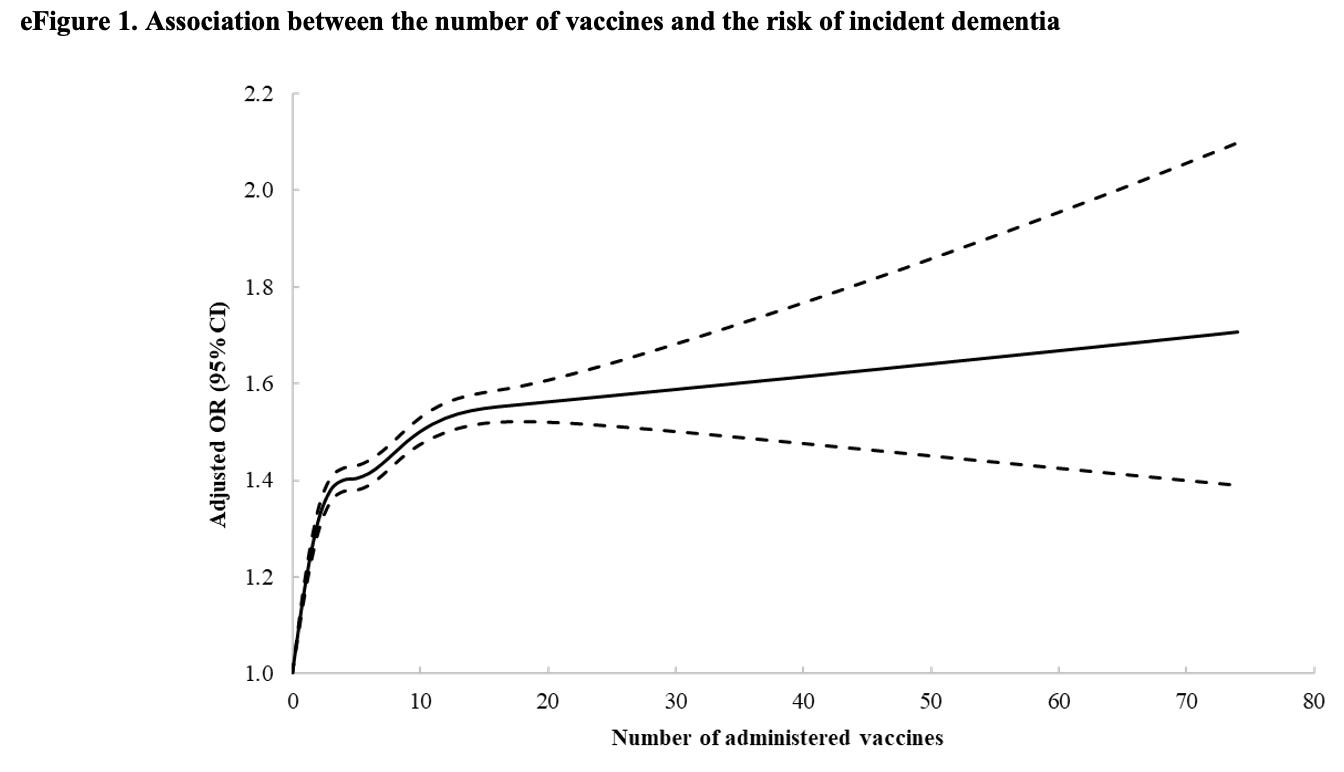
The authors ran multiple dose–response models, and every one of them shows the same pattern:
From eTable 2:
From eTable 7:
This is one of the most powerful and unmistakable signals in epidemiology.

Another signal strongly inconsistent with mere bias: a time-response relationship.
The highest dementia risk occurs 2–4.9 years after vaccination (Adjusted OR 1.56). The risk then slowly attenuates but never returns to baseline, remaining elevated across all time windows.
After 12.5 years, the risk is still meaningfully elevated (Adjusted OR 1.28) — a persistence incompatible with short-term “detection bias” and suggestive of a long-lasting biological impact.
This pattern is what you expect from a biological trigger with long-latency neuroinflammatory or neurodegenerative consequences.
When the authors apply a long 10-year lag — meant to eliminate early detection bias — the elevated risk persists:
If this were simply “people who see doctors more often get diagnosed earlier,” the association should disappear under long lag correction.
Two vaccines show particularly strong associations:
And again, both exhibit dose–response escalation — the hallmark pattern of a genuine exposure–outcome relationship.
Taken together, the findings across primary, supplemental, dose–response, time–response, stratified, and sensitivity analyses paint the same picture:
This is what a robust epidemiologic signal looks like.
In the largest single study ever conducted on vaccines and dementia, common adult vaccinations were associated with a 38% higher risk of dementia and a 50% higher risk of Alzheimer’s disease. The risk increases with more doses, persists for a decade, and is strongest for influenza and pneumococcal vaccines.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
